Avoiding Falls In Public and at Home
Avoiding falls in public is crucial for seniors to maintain their safety and independence. Here are some practical tips to help prevent falls and reduce the risk of injury:
1. Wear Proper Footwear:
- Supportive Shoes: Choose shoes with good arch support, non-slip soles, and a secure fit. Avoid wearing high heels, flip-flops, or slippery-soled shoes.
- Avoid Slippers: Avoid wearing slippers or loose shoes outside, as they can increase the risk of tripping.
2. Use Assistive Devices:
- Walking Aids: Use a cane, walker, or other mobility aids if needed. Make sure these devices are properly adjusted and maintained.
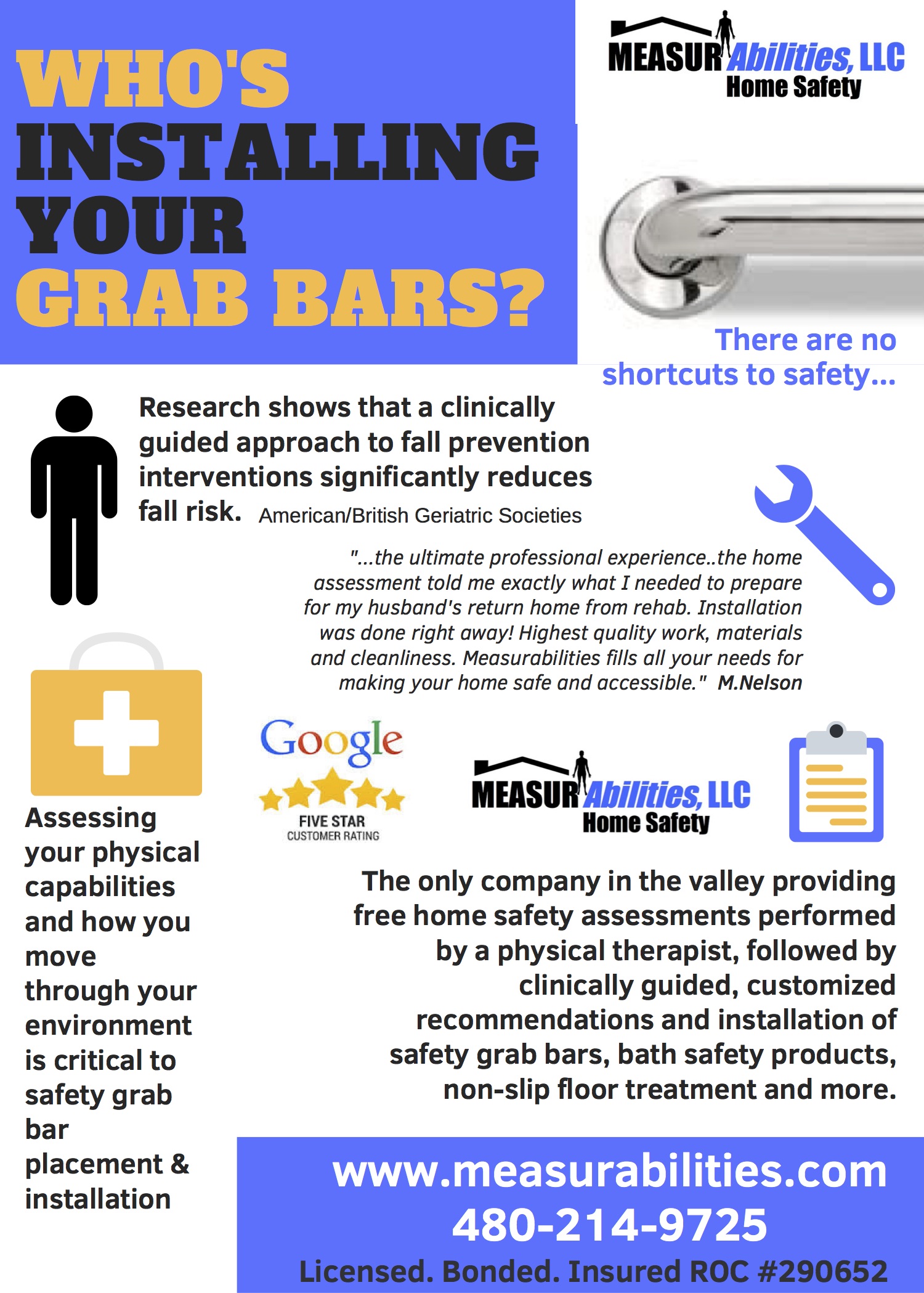
- Grab Bars: Install grab bars in strategic places at home, such as near stairs and in the bathroom.
3. Be Mindful of Your Surroundings:
- Watch Your Step: Pay attention to the ground and any potential hazards like uneven surfaces, potholes, or curbs.
- Avoid Obstacles: Stay clear of obstacles such as outdoor furniture, signs, or other items that might be in your path.
4. Improve Balance and Strength:
- Exercise Regularly: Engage in exercises that improve balance, strength, and flexibility, such as Tai Chi, yoga, or specific balance training exercises.
- Strength Training: Incorporate strength training exercises to maintain muscle strength, which can help with stability.
5. Stay Hydrated and Nourished:
- Hydration: Drink plenty of water, as dehydration can lead to dizziness and an increased risk of falling.
- Balanced Diet: Maintain a balanced diet rich in calcium and vitamin D to support bone health and prevent falls.
6. Plan Your Outings:
- Daylight: Whenever possible, plan to go out during daylight hours to improve visibility and avoid walking in low light.
- Accompanied Travel: If possible, travel with a companion who can assist you if needed.
7. Use Safety Features:
- Handrails: Utilize handrails on stairs and ramps. Ensure that they are sturdy and securely installed.
- Well-Lit Areas: Choose well-lit routes and avoid poorly lit areas to reduce the risk of tripping or missing steps.
8. Monitor Health and Medication:
- Regular Check-Ups: Have regular check-ups with your healthcare provider to monitor health conditions that may affect balance, such as vision or inner ear issues.
- Medication Review: Review medications with your doctor, as some medications may cause dizziness or affect balance.
9. Practice Safe Walking Techniques:
- Slow and Steady: Walk slowly and carefully, especially when navigating uneven surfaces or obstacles.
- Focus: Keep your focus on where you’re walking rather than looking around or using your phone.
10. Use Fall Prevention Programs:
- Community Programs: Participate in fall prevention programs offered by local community centers or health organizations. These programs often include exercises and education to help reduce fall risk.
11. Emergency Preparedness:
- Emergency Contact: Carry a phone or an emergency alert device to call for help if you do fall or need assistance.
- Medical Alert System: Consider using a medical alert system that allows you to call for help quickly if needed.
By incorporating these strategies into daily routines, seniors can significantly reduce their risk of falling in public and maintain greater confidence and safety while moving about.
Falls are a major cause of injuries and death among older adults. Here are some tips to help you avoid falls at home:
- Make sure your home is well-lit. This will help you see where you are going and avoid tripping over objects.
- Remove clutter from walkways. This will also help you avoid tripping.
- Secure loose rugs and carpets. Loose rugs and carpets can be a tripping hazard. Secure them with double-sided tape or tacks.
- Install grab bars in the bathroom and near stairs. Grab bars can help you steady yourself when you are getting up or down.
- Use a cane or walker if you need one. A cane or walker can provide you with extra support and help you avoid falls.
- Wear comfortable shoes that fit well. Shoes that are too loose or too tight can make you more likely to trip.
- Get regular exercise. Exercise can help improve your balance and coordination, which can help you avoid falls.
- Get your vision checked regularly. Poor vision can make it more difficult to see where you are going, which can increase your risk of falls.
- Take your time. Don’t rush when you are walking or moving around. Take your time and be careful.
- Tell your doctor if you have any balance or mobility problems. Your doctor can help you develop a plan to prevent falls.
If you have fallen in the past, it is important to take steps to prevent future falls. Talk to your doctor about your risk of falls and get help developing a plan to stay safe.
Here are some additional tips for older adults:
- Get up and move around regularly. Don’t sit or lie down for long periods of time.
- Stay hydrated. Dehydration can make you dizzy and more likely to fall.
- Eat a healthy diet. A healthy diet can help you maintain a healthy weight, which can reduce your risk of falls.
- Manage your chronic conditions. Conditions such as arthritis, heart disease, and diabetes can increase your risk of falls. Make sure to manage these conditions under the guidance of your doctor.
- Stay mentally active. Mental activity can help improve your balance and coordination.
- Stay socially active. Social activity can help reduce stress, which can also increase your risk of falls.
By following these tips, you can help reduce your risk of falls and stay safe at home.
There are many comfortable shoes for seniors on the market, but some of the most popular include:
- Walking shoes: Walking shoes are designed to provide support and comfort for walking. They typically have cushioned soles and arch support.
- Running shoes: Running shoes are designed for high-impact activities like running. They typically have more cushioning than walking shoes and may also have features to prevent ankle rolling.
- Trail shoes: Trail shoes are designed for walking or hiking on uneven surfaces. They typically have good traction and durability.
- Diabetic shoes: Diabetic shoes are designed for people with diabetes. They typically have features to help prevent foot ulcers, such as extra width and cushioning.
- Comfort shoes: Comfort shoes are designed to be as comfortable as possible. They may have features such as memory foam or gel inserts.
When choosing comfortable shoes for seniors, it is important to consider the following factors:
- The person’s foot type: Some people have wider feet, while others have narrower feet. It is important to choose shoes that fit the person’s foot type well.
- The person’s activity level: If the person is active, they will need shoes that provide more support and cushioning. If the person is less active, they may be able to get away with shoes that are less supportive.
- The person’s budget: There are a variety of comfortable shoes available at different price points. It is important to choose shoes that fit the person’s budget.
It is also important to have the shoes fitted by a qualified professional, such as a podiatrist or an orthotist. This will help ensure that the shoes provide the correct amount of support and comfort.
Here are some additional tips for choosing comfortable shoes for seniors:
- Try on the shoes at the end of the day: Your feet tend to swell throughout the day, so it is important to try on shoes at the end of the day when your feet are at their largest.
- Walk around in the shoes: Don’t just stand in the shoes when you try them on. Walk around in them to make sure they are comfortable and provide good support.
- Bend your knees: When you bend your knees, the shoes should not feel too tight.
- Have the salesperson check the fit: The salesperson should be able to check the fit of the shoes and make sure they are not too tight or too loose.
Balance issues are common in older adults. They can be caused by a variety of factors, including:
- Age-related changes in the inner ear: The inner ear is responsible for balance, and it can start to decline with age.
- Vision problems: Poor vision can make it difficult to see where you are going, which can lead to balance problems.
- Dehydration: Dehydration can make you dizzy and more likely to fall.
- Medications: Some medications can cause dizziness or drowsiness, which can increase the risk of falls.
- Medical conditions: Medical conditions such as arthritis, diabetes, and Parkinson’s disease can also increase the risk of balance problems.
Balance problems can lead to falls, which are a major cause of injuries and death in older adults. If you are a senior, it is important to take steps to prevent balance problems and falls.
Here are some tips for preventing balance problems in seniors:
- Get regular exercise: Exercise can help improve balance and coordination.
- Wear comfortable shoes that fit well: Shoes that are too loose or too tight can make you more likely to trip.
- Make sure your home is well-lit: This will help you see where you are going and avoid tripping over objects.
- Remove clutter from walkways: This will also help you avoid tripping.
- Secure loose rugs and carpets: Loose rugs and carpets can be a tripping hazard. Secure them with double-sided tape or tacks.
- Install grab bars in the bathroom and near stairs: Grab bars can help you steady yourself when you are getting up or down.
- Use a cane or walker if you need one: A cane or walker can provide you with extra support and help you avoid falls.
- Get your vision checked regularly: Poor vision can make it more difficult to see where you are going, which can increase your risk of falls.
- Take your time: Don’t rush when you are walking or moving around. Take your time and be careful.
- Tell your doctor if you have any balance or mobility problems: Your doctor can help you develop a plan to prevent falls.
If you have fallen in the past, it is important to take steps to prevent future falls. Talk to your doctor about your risk of falls and get help developing a plan to stay safe.